Antibiotic therapy for uncomplicated urinary tract infections (UTIs) caused by Escherichia coli.
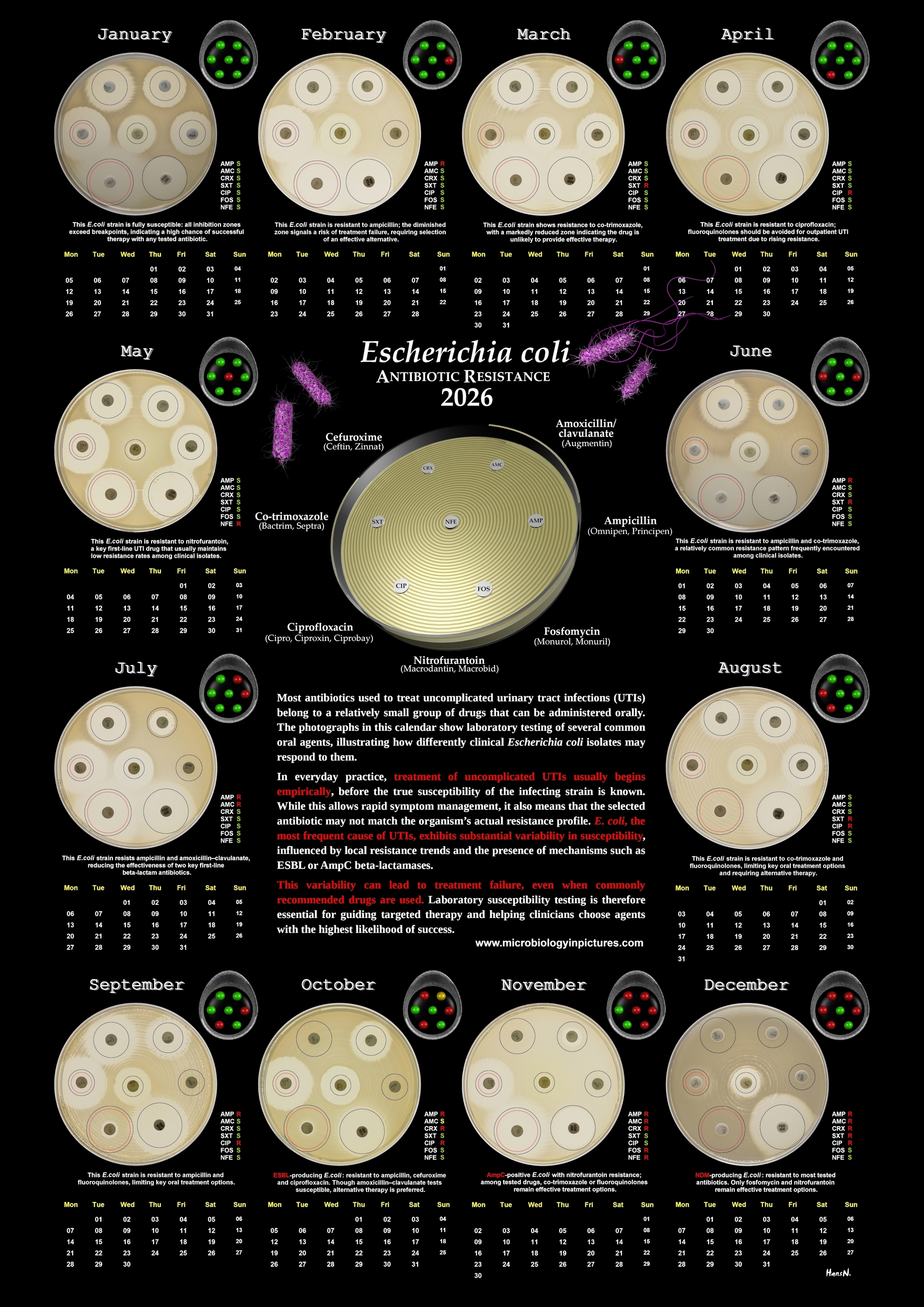
Antibiotic therapy for uncomplicated urinary tract infections (UTIs) relies heavily on a relatively small group of antibiotics that are available for oral administration. The photographs in this calendar illustrate laboratory testing of several commonly used oral agents, highlighting the diversity of susceptibility patterns found among clinical Escherichia coli isolates. Because the range of orally applicable antibiotics is limited, choosing an effective treatment can be challenging—especially as resistance continues to rise worldwide.In routine clinical practice, treatment for uncomplicated UTIs is often initiated empirically, meaning that therapy begins before laboratory results are available. While this approach is necessary to provide timely care, it also carries risk: the antibiotic selected may not match the actual susceptibility profile of the infecting strain.
E. coli, the primary causative agent of UTIs, displays considerable variability in its resistance patterns. Even within the same community or healthcare setting, isolates may differ significantly in their susceptibility to key oral antibiotics such as ampicillin, amoxicillin/clavulanate, co-trimoxazole, fluoroquinolones, fosfomycin, nitrofurantoin, or oral cephalosporins. This natural heterogeneity means that empirical therapy may sometimes fail, particularly when resistance rates for a given agent are high or when the infecting strain expresses specific resistance mechanisms, such as NDM, ESBL or AmpC beta-lactamases.
Laboratory testing therefore plays a critical role in guiding targeted treatment, improving the likelihood of clinical success, and supporting antimicrobial stewardship efforts. By presenting twelve real examples of susceptibility testing across different antibiotic profiles, this calendar aims to increase awareness of the challenges associated with oral antibiotic selection for UTIs. Understanding the limits of empirical therapy and the importance of resistance monitoring is essential not only for clinicians, but for anyone interested in the growing global issue of antimicrobial resistance.
