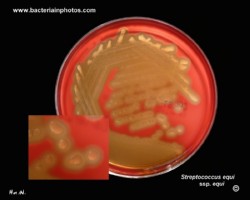
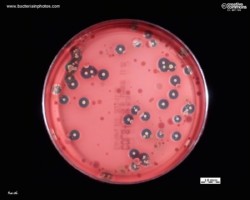
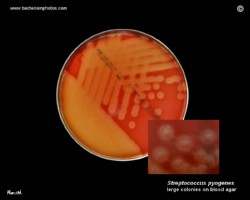
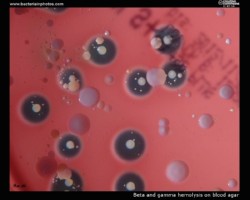
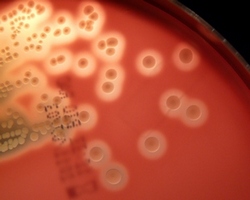
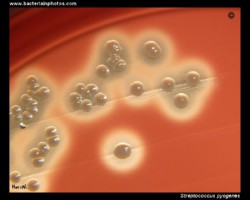
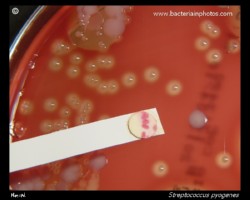
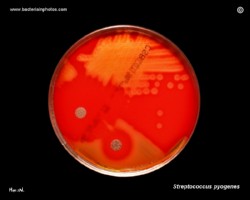
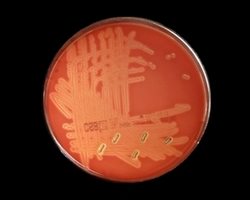
Streptococci grow best in media enriched with digest of animal tissues and defibrinated blood (usually sheep or horse). On blood agar plates they form colonies ranging from pinpoint size to 2-3 mm in diameter after 24 hours. A distinctive feature of streptococcal growth on blood agar is the production by many species of alpha- or beta-hemolysis. Hemolysis is dependent on several cultural features, including the species of blood used and the incubation atmosphere. It was recognized early that pathogenic streptococci for the most part fell in the beta-hemolytic category.
Beta-hemolysis appears as complete clearing of the medium. The size, the distinctness and the rate of development of the zone of beta-hemolysis surrounding colonies vary considerably. Some strains produce unusually large and brilliant zones, while others may show no more than a narrow ring of hemolysis surrounding the colony.
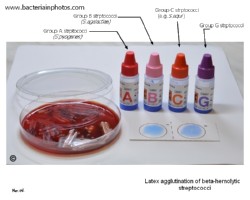
Majority of pathogenic streptococci possess specific carbohydrate antigens, which permit the classification of streptococci into groups. The presence of these antigens is demonstrated by means of precipitin reactions between solutions of the carbohydrate extracted from streptococcal cells and antisera prepared by immunizing rabbits with heat-killed suspensions of streptococci. Rebecca Lancefield showed that separating hemolytic streptococci into distinct categories by this technic resulted in a classification related to the most characteristic source of the organisms. Although group A (S.pyogenes) and group B (S.agalactiae) strains are responsible for most human streptococcal infections, occasionally representatives of all other groups may be isolated from human sources.
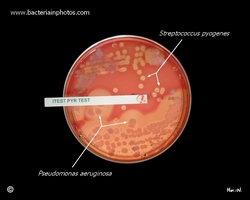
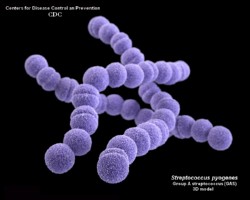
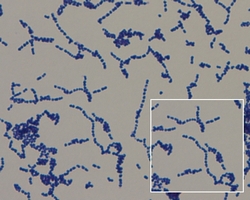
Streptococcus pyogenes
Group A beta-hemolytic streptococci (GAS)
Beta-hemolysis is caused by streptolysin S and the oxygen-labile streptolysin O (both of which are produced by most S.pyogenes strains). Beta-hemolysis by streptolysin O occurs only under anaerobic conditions. Streptococcus pyogenes can cause a variety of acute pyogenic infections. One of the most common bacterial infections is streptococcal pharyngitis. The illness is characterized by acute sore throat, fever, an headache. The condition can be indistinguishable from viral pharyngitis (streptococcal pharyngitis can only be diagnosed by demonstrating the presence of the organism with laboratory tests).





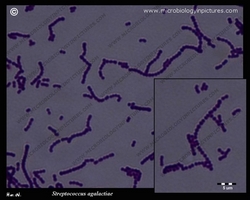
Streptococcus agalactiae
Group B beta-hemolytic streptococci (GBS)
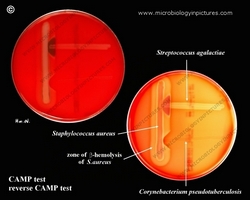
In comparison of those of group A strains, the colonies produced on blood agar are usually larger and may show yellow to orange pigments with anaerobic incubation. Beta-hemolysis is less distinct and may be absent, particularly under aerobic conditions.
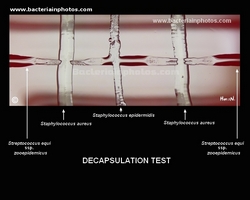
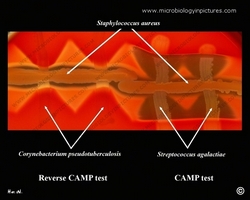
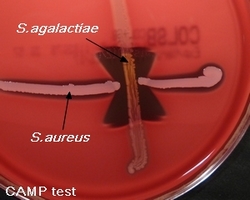
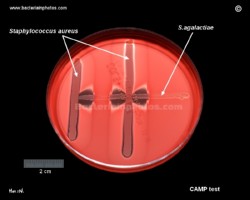
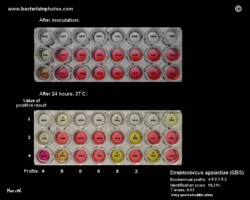
The majority of group B sreptococci produce a diffusable extracellular protein that acts synergisically with staphylococcal beta lysin to lyse erythrocytes (CAMP factor). A positive test is characterized by an arrowhead-shaped zone of complete hemolysis in the area into which both staphylococcal beta lysin and CAMP factor have diffused. Definitive identification involves serologic determination of Lancefield group.
GBS is an asymptomatic (presenting no symptoms of disease) colonizer of the gastrointestinal human tract. Nevertheless, this opportunistic harmless bacterium can, in some circumstances, cause severe invasive infections.
Although GBS colonization usually does not cause problems in healthy women during pregnancy, it can sometimes cause serious illness for the mother and is the leading cause of bacterial neonatal infection in the baby during gestation and after delivery with significant mortality rates in premature infants.
Group B streptococci are susceptible to the same antimicrobials as group A organisms, however , they are less susceptible to penicillin G and more frequently resistant to tetracycline and other antibiotics.




Streptococcus equi
Group C beta-hemolytic streptococci
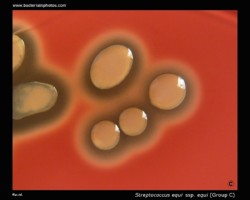
Streptococcus equi is a Gram-positive bacterium of the Lancefield's group C. It grows in long chains of irregularly shaped cocci that are nonmotile. Streptococcus equi ssp.equi is the etiologic agent for the upper respiratory disease in horses commonly referred to as strangles. Colonies of virulent S.equi are always mucoid.
Streptococcus equi ssp. zooepidemicus is a commensal of horses, and its host range also includes swine, cattle, poultry, rabbits and human.
It's a clonal ancestor of S. equi with which shares greater than 98% DNA homology and many of the virulence factors. It occasionally causes human infection that can be traced back to contact with horses or consumption
of unpasteurized dairy products. Unlike S.equi ssp.equi, S.equi ssp. zooepidemicus ferments sorbitol and lactose.
In the process of fermentation S. zooepidemicus produces hyaluronic acid as a component of its extracellular capsule.